Does Medicare Require A Prior Authorization . prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. However, to contain costs, the centers. original medicare requires prior authorization only for three types of services. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. In 2022, most of the requests were approved in an average of. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. medicare rarely requires prior authorizations.
from mavink.com
prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. original medicare requires prior authorization only for three types of services. medicare rarely requires prior authorizations. However, to contain costs, the centers. In 2022, most of the requests were approved in an average of. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get.
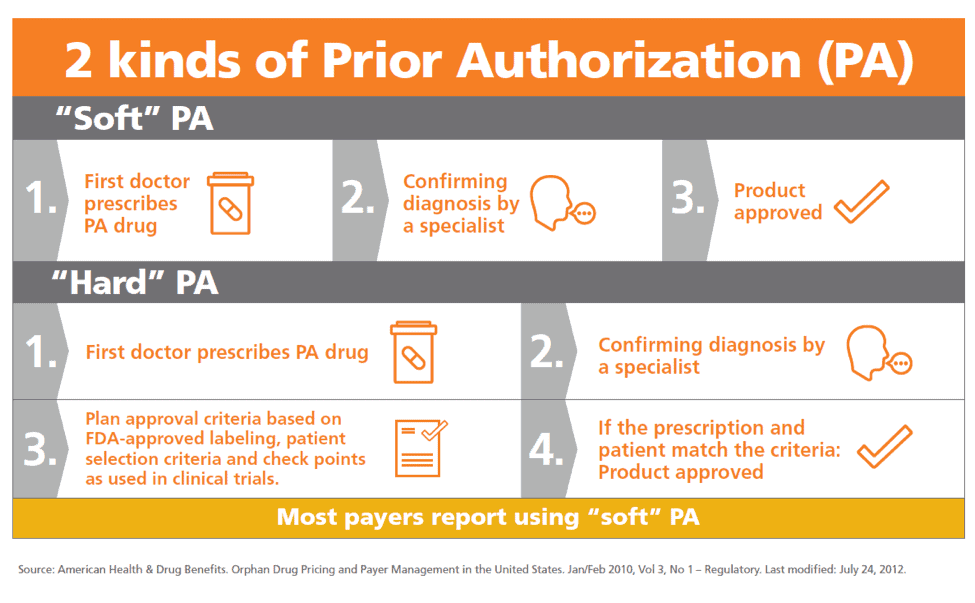
Prior Authorization Process Flow Chart
Does Medicare Require A Prior Authorization If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. However, to contain costs, the centers. medicare rarely requires prior authorizations. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. In 2022, most of the requests were approved in an average of. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. original medicare requires prior authorization only for three types of services.
From slideplayer.com
UC Retiree Health and Medicare ppt download Does Medicare Require A Prior Authorization prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. However, to contain costs, the centers. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. medicare rarely. Does Medicare Require A Prior Authorization.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word Does Medicare Require A Prior Authorization However, to contain costs, the centers. prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. original medicare requires prior authorization only for three types of services. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. In 2022, most of the. Does Medicare Require A Prior Authorization.
From themedicarefamily.com
Does Medicare Require Prior Authorization? Does Medicare Require A Prior Authorization original medicare requires prior authorization only for three types of services. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. cms believes prior authorization for certain hospital opd services will. Does Medicare Require A Prior Authorization.
From mavink.com
Prior Authorization Process Flow Chart Does Medicare Require A Prior Authorization If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. medicare rarely requires prior authorizations. original medicare requires prior authorization only for three types of services. prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given. Does Medicare Require A Prior Authorization.
From www.slideshare.net
Prior Authorizations for Medications an Overview Does Medicare Require A Prior Authorization However, to contain costs, the centers. prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. In 2022, most of the requests were approved in an average of. original medicare requires prior authorization only for. Does Medicare Require A Prior Authorization.
From specialty-health.blogspot.com
Specialty Health What Is Prior Authorization For Medication Does Medicare Require A Prior Authorization original medicare requires prior authorization only for three types of services. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. cms believes prior authorization for certain hospital opd services will ensure that medicare. Does Medicare Require A Prior Authorization.
From exorcsbbl.blob.core.windows.net
Wv Medicare Prior Authorization Form at Linda Beaudoin blog Does Medicare Require A Prior Authorization prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get.. Does Medicare Require A Prior Authorization.
From www.phoenixvirtualstaff.com
The Complete Guide to Prior Authorization Navigating the Complex Does Medicare Require A Prior Authorization original medicare requires prior authorization only for three types of services. In 2022, most of the requests were approved in an average of. However, to contain costs, the centers. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. If you have a medicare advantage plan and need to see a specialist not in your. Does Medicare Require A Prior Authorization.
From www.youtube.com
Prior Authorization How do you get insurance companies to approve Does Medicare Require A Prior Authorization the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. original medicare requires prior authorization only for three types of services. prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. In 2022, most of the requests were approved in an average of. If you. Does Medicare Require A Prior Authorization.
From medicare-faqs.com
How To Do A Prior Authorization For Medicare Does Medicare Require A Prior Authorization medicare rarely requires prior authorizations. original medicare requires prior authorization only for three types of services. However, to contain costs, the centers. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. In 2022, most of the requests were approved in an average of. the prior authorization program for certain. Does Medicare Require A Prior Authorization.
From whatismedicaresurtaxreharui.blogspot.com
What Is Medicare Surtax Prior Authorization For Medication For Medicare Does Medicare Require A Prior Authorization prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. original medicare requires prior authorization only for three types of services. medicare rarely requires prior authorizations. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to. Does Medicare Require A Prior Authorization.
From dodiqclaribel.pages.dev
2024 Prior Authorization State Law Chart Erinna Karlyn Does Medicare Require A Prior Authorization original medicare requires prior authorization only for three types of services. However, to contain costs, the centers. medicare rarely requires prior authorizations. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to. Does Medicare Require A Prior Authorization.
From www.youtube.com
Medicare Advantage Plans Require Prior Authorization!!! YouTube Does Medicare Require A Prior Authorization original medicare requires prior authorization only for three types of services. prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. the prior authorization program. Does Medicare Require A Prior Authorization.
From www.formsbank.com
Molina Healthcare Medicaid And Medicare Prior Authorization Request Does Medicare Require A Prior Authorization medicare rarely requires prior authorizations. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. original medicare requires prior authorization only for three types of services. However, to contain costs, the centers. In 2022, most of the requests were approved in an average of. If you have a medicare advantage plan and need to. Does Medicare Require A Prior Authorization.
From portiva.com
Does Medicare Require Prior Authorization Medicare FAQs Does Medicare Require A Prior Authorization medicare rarely requires prior authorizations. original medicare requires prior authorization only for three types of services. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. prior authorization is a. Does Medicare Require A Prior Authorization.
From versalushealth.com
Medicare Update Prior Authorization Request Process for Certain Does Medicare Require A Prior Authorization cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. medicare rarely requires prior authorizations. However, to contain costs, the centers. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. original medicare requires prior authorization only for. Does Medicare Require A Prior Authorization.
From www.healthleadersmedia.com
How Prior Authorization in Medicare Advantage is Harming Everyone Does Medicare Require A Prior Authorization prior authorization is a requirement that a health care provider obtain approval from medicare to provide a given service. However, to contain costs, the centers. In 2022, most of the requests were approved in an average of. original medicare requires prior authorization only for three types of services. medicare rarely requires prior authorizations. If you have a. Does Medicare Require A Prior Authorization.
From www.aiohotzgirl.com
Free Medicare Prior Rx Authorization Form Pdf Eforms Free Download Does Medicare Require A Prior Authorization the prior authorization program for certain hospital opd services ensures that medicare beneficiaries. cms believes prior authorization for certain hospital opd services will ensure that medicare beneficiaries continue to. If you have a medicare advantage plan and need to see a specialist not in your plan’s network, you may have to get. prior authorization is a requirement. Does Medicare Require A Prior Authorization.